Light-based drug delivery systems use nanoparticles that respond to specific light wavelengths, usually near-infrared, to release drugs exactly where you need them. These tiny particles target diseased cells, absorb the light energy, and convert it into heat, triggering drug release while minimizing damage to healthy tissues. This approach offers precise control, reduces side effects, and improves treatment outcomes. To discover how this innovative technology is shaping future therapies, keep exploring its exciting potential.
Key Takeaways
- Nanoparticles can be engineered to target specific disease markers for precise drug delivery.
- Light, especially near-infrared, activates nanoparticles to release drugs selectively at disease sites.
- Photothermal activation allows controlled, on-demand drug release with minimal damage to healthy tissues.
- This system enhances treatment efficacy by combining thermal destruction with targeted drug delivery.
- Ongoing research aims to improve safety, accessibility, and minimize allergy risks of light-based delivery methods.
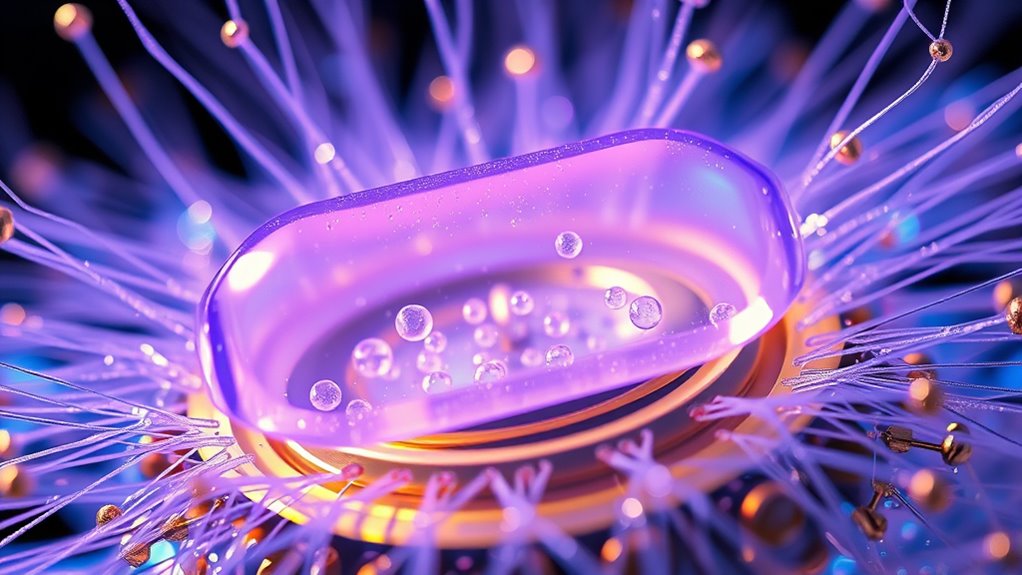
Have you ever wondered how light can be used to deliver drugs precisely where they’re needed? It’s a fascinating area of research that combines physics, chemistry, and medicine to develop smarter treatments. One of the key techniques involves nanoparticle targeting, where tiny particles are engineered to seek out specific cells or tissues. These nanoparticles are often designed with surface molecules that recognize and bind to markers unique to cancer cells or other diseased tissues. When these targeted nanoparticles are introduced into your body, they travel through the bloodstream and hone in on their designated sites, minimizing damage to healthy tissue. This approach enhances drug efficacy while reducing side effects, making treatments more effective and tolerable.
Once the nanoparticles reach their target, light comes into play through a process called photothermal activation. When you shine a specific wavelength of light—often near-infrared—on these nanoparticles, they absorb the light energy and convert it into heat. This localized heating effect can trigger the release of the drug payload directly at the disease site. Because the heat is confined to the nanoparticle area, it minimizes collateral damage to surrounding healthy tissue. This method not only ensures the drug acts precisely where it’s needed but also offers a way to control the timing of drug release. You can activate the treatment on demand by applying light, giving you a high degree of control over therapy.
Light-triggered heat release enables precise, on-demand drug delivery with minimal damage to healthy tissue.
The combination of nanoparticle targeting and photothermal activation opens up many possibilities. For instance, it allows you to treat tumors that are difficult to reach with conventional methods. By injecting targeted nanoparticles and then using a laser to activate them, you can achieve high local drug concentrations without affecting the entire body. Additionally, the heat generated can help destroy cancer cells directly, providing a dual attack—both from the drug and the thermal effect. This synergy boosts treatment effectiveness and can even overcome some forms of drug resistance.
In essence, light-based drug delivery systems harness the precision of nanoparticle targeting and the controllability of photothermal activation to revolutionize how we approach disease treatment. It’s a promising avenue that could lead to therapies with fewer side effects, greater precision, and improved outcomes. As research advances, you’ll likely see these techniques becoming more refined and accessible, transforming the way you think about medicine and personalized treatment. Furthermore, understanding the allergy risks associated with some nanoparticle components is important for ensuring patient safety during these innovative therapies.
Frequently Asked Questions
How Do Light-Based Systems Target Specific Cell Types?
You achieve cell specificity in light-based systems by using targeting strategies like attaching light-sensitive molecules or nanoparticles to specific cell markers. When exposed to certain wavelengths, these systems activate and deliver drugs precisely where needed. This approach minimizes side effects, maximizes treatment efficiency, and guarantees that only the targeted cells receive the therapeutic agents, making your treatment more effective and personalized.
What Are the Long-Term Safety Concerns?
Like a double-edged sword, light-based systems promise precision but pose safety concerns. You should worry about biocompatibility issues and long-term toxicity, as persistent exposure might cause tissue damage or immune responses. While current studies are promising, long-term effects remain uncertain, making it essential to monitor safety closely. Ensuring these systems are safe over extended periods is key to their successful, widespread adoption.
Can Light Activation Control Drug Release Duration?
Yes, light activation can control drug release duration through photothermal effects, which generate localized heat to trigger drug release precisely. By adjusting light intensity and exposure time, you can fine-tune the release rate, ensuring accurate delivery. This photoactivation precision allows you to manage how long the drug is released, providing personalized treatment options and reducing side effects, making light-based systems highly adaptable for therapeutic needs.
Are There Limitations in Light Penetration Depth?
Sure, light penetration depth is a real party pooper. Thanks to tissue scattering and light attenuation, your precious photons can’t travel far, limiting effective drug delivery to superficial tissues. Ironically, the more you need deep reach, the more you realize light’s not quite the superhero it’s made out to be. So, if you’re hoping for deep tissue access, you’ll need to get creative or settle for surface-level solutions.
How Do These Systems Compare Cost-Wise to Traditional Methods?
You’ll find that light-based drug delivery systems can be more expensive initially due to cost analysis and manufacturing challenges. They often require specialized equipment and materials, increasing production costs. However, over time, they may reduce overall healthcare expenses by improving targeting accuracy and minimizing side effects. While the upfront costs are higher, the potential for more efficient treatments could justify the investment compared to traditional methods.
Conclusion
Remember, the early bird catches the worm, and with light-based drug delivery systems, you’re pioneering a precise, non-invasive approach to medicine. By harnessing light, you can target treatments exactly where needed, minimizing side effects. As technology advances, you’ll find more ways to improve patient outcomes and revolutionize healthcare. Stay ahead of the curve—because in this field, innovation shines brightest when you seize the opportunity now.